Gluteal tendinopathy explained – symptoms, exercises and more
Tue,Jan 02, 2018 at 04:30PM by Carla Mullins
Gluteal tendinopathy and why it’s “Love me tendon…”
Using an unashamed pun from Elvis and his classic song Love me Tender, our article Love me Tendon explains gluteal tendinopathy, its pathology and its symptoms. It also provides exercises and great ideas on programs for recovery and rehabilitation. And your clients will love the improvements to their glute med tendinopathy!
This blog is an introduction to the concepts of tendinopathy and also the pelvis. If you are wanting to learn more about the concepts we suggest you try some of our online on-demand courses.
Gluteal tendinopathy and its associated lateral hip pain is the most common form of hip tendonitis or hip tendon injury. Gluteal tendinopathy is also known as gluteus medius tendinopathy (glute med tendinopathy), gluteal tendinitis or even gluteus medius tendinosis.
Explaining tendons and their functions – using a horse and cart analogy
Tendons are perhaps the anatomical equivalent of the middle child; they do a lot of work holding things together, but aren’t talked about as much as the first born (the bones) and the youngest (the ligaments).
Scientifically speaking, a tendon is flexible but tough fibrous band of connective tissue that is responsible for attaching muscle to bone.
From a functional point of view, I like to explain tendon issues to clients by relating it to a horse and cart. Let’s elaborate:
// The horse represents our muscles. The horse provides the power for movement;
// The cart represents our skeletal system and the load for the muscles (the horse) to pull;
// The ropes and bridle that attach the horse to the cart are our tendons. As such, the tendons need to have good integrity in order to distribute power evenly when moving a load.
When moving, we want to ensure that the cart (skeleton) moves as efficiently as possible. For this to occur, all three of the aforementioned elements need to be working together.
From a pilates perspective this really highlights the importance of applying the pilates principles:
// Alignment of the skeleton;
// Control of muscle and tendon as they work through their range of motion (ROM);
// Precision of movement.
Exercise is considered a good method for treating tendon-related issues (Cook & Purdham 2009). Having an understanding of the presenting tendon issue and, therefore, the appropriate type of exercise to administer is key to optimal recovery. In this article we will look at:
// What is a tendinopathy?
// Gluteal tendinopathy and the relationship with greater trochanteric bursitis;
// Load, progression and the continuum;
// Protocol for tendon repair – staging;
// How to get the best result for individual clients from a pilates perspective.
What is a tendinopathy?
Put simply, the term tendinopathy describes the clinical conditions associated with overuse in and around tendons.
Tendons can be damaged at the:
// Insertion point to the bone;
// Belly of the tendon;
// Attachment point to the muscle.
Tendon pathology has been described as a continuum (Cook & Purdam 2009) with three distinct stages:
// Reactive tendinopathy;
// Tendon disrepair;
// Degenerative tendinopathy.
From a pilates and exercise perspective, it is important to note that load is considered to be the primary stimulus which drives tendon health forward and back along the continuum.
// Low load will result in the tendon decreasing in size or furthering into degeneration;
// High load will result in inflammation or further tendon degeneration;
// The “Goldilocks Zone” will result in tendon growth and repair.
Pain response to loading is the current gold standard for measuring what load is suitable for a particular stage of degeneration. The table below illustrates how load can help to create a healthy tendon response, with the “Goldilocks Zone” marked A.
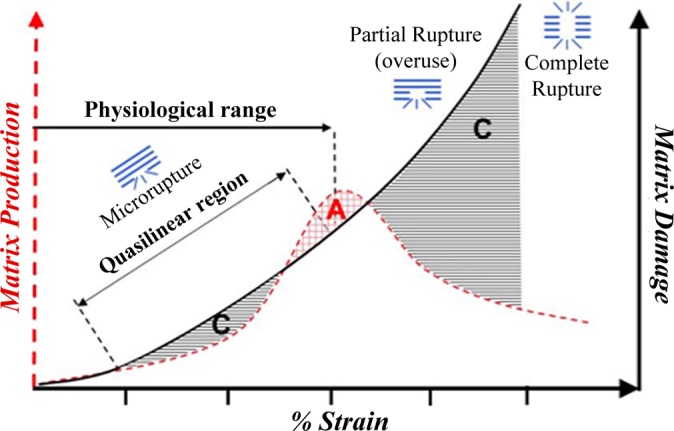
Source: Orthopaedic Journal of Sports Medicine (Nov 2016)
Gluteal tendinopathy and the relationship with greater trochanteric bursitis
Traditionally it has been thought that greater trochanteric bursitis and gluteal tendinopathy were a team of pathologies. However, research by people such as Dr Alison Grimaldi indicate that the greater trochanter bursitis element is probably better described as lateral hip pain that can be attributable to compressive forces such as lying on your side or the collapse into the hip when standing on one leg (see image below).

An example of poor pelvic control
For those wanting to read more on this topic I suggest you read the article Lateral Hip Pain: Mechanisms and Management by Dr Alison Grimaldi.
Load, progression and the continuum
Within the constraints of recovery proposed by Cook & Purdam (2009), relative rest or load adjustment may allow the tendon to return to a previous level of structure and capacity within the continuum.
When a physiotherapist discusses load they will consider a number of factors:
Exercise type
// Open versus Closed chain;
// Eccentric versus Concentric;
// Isometric versus Dynamic;
// Number of repetitions;
// Degree of resistance.
Stage of disrepair
// Degenerative tendinopathies will react better to eccentric exercise based intervention. Tendons respond better to work than rest
Pharmacotherapies
// Therapy using pharmaceutical drugs, as distinguished from therapy using surgery, radiation, movement;
// Examples are NSAIDS or pain medication.
When working with a physiotherapist, a movement teacher and client need to be aware of these considerations and how they are going to affect decisions about the staging of movement and exercise in order to achieve tendon repair and balanced movement.
Staging and a protocol for tendon repair
Staging of the appropriate load in exercises and movements is an important aspect of tendon recovery. A decision is made on how load-tolerant a tendon would be includes an identification of where the person is within these stages:
// Stage One: Is the person presenting as intolerant to load, i.e. are they showing a painful response to any load?
// Stage Two: Is the person presenting as load tolerant, i.e. manages to achieve a positive response to slow speed and high load, e.g. standing on one leg?
// Stage Three: Is the person presenting as load tolerant to fast speed and high load (energy storage) e.g. walking?
Being specific with the appropriate degree of load can become an art form, as there are many factors individual to each person to consider. Factors such as fear, pain, apprehension and inflammatory response may all affect the person’s ability to transit from one stage to the next.
When working with tendon pathology we need to appreciate there are stages to recovery specific to the muscle and tendon affected. Accordingly, we need to identify the staging for that muscle and tendon and incorporate this into the appropriate steps of a pilates program.
Below are some of the specific exercises that would be incorporated into each stage of tendon repair for glute med tendinopathy. Remembering that the focus in these cases are the specific muscles and tendons of this pathology. As a result this focus would be about 20 minutes of work in an hour program. The whole program, ideas for which are discussed later in this article, would be looking at the broader patterning and movement of the individual. I like to think that when dealing with a pathology we have to still make sure we are dealing with that in the context of the person and their patterns.
Step One: Isometric with increasing load
a) Side lying single leg hover in neutral;
b) Single leg stance;
c) Single leg stance + resisted abduction;
d) Hoof;
e) Scooter;
f) Single leg stance plus free form disc;
g) Single leg stance, Wunda chair push down.
Step Two: Dynamic – high load, low speed
a) Lunges;
b) Assisted squat (Ped-O-Pull or Sling);
c) Assisted single leg squat (Ped-O-Pull);
d) Wunda Chair step-up;
e) Arabesque;
f) Side lying reformer;
g) CoreAlign – resisted abduction.
Step Three: Dynamic – high load, high speed
(any of Step Two but with higher speed)
a) Free form lunges;
b) Jump board on Reformer;
c) Bosu ball step up;
d) Bosu ball single leg squat;
e) Single leg hip hitching.
Step Four: Sport specific drills
a) Side stepping, sprinting;
b) Jump and land.
What is progression from a pilates perspective?
From a pilates standpoint there are processes of progression. We are dealing with the person, not just the pathology.
// We start in the most stable position, e.g. double leg work on the Reformer;
// We then add challenge to stability, e.g. to challenge pelvic stability we might progress by performing pelvic press on the Wunda Chair, shoulder bridge on the Wunda Chair.
In essence, we are aiming to improve muscular alignment in order to achieve an efficient and balanced body. It is important for us to remember this, particularly when working with clients who have specific pathologies such as gluteal tendinopathy.
// The load challenge occurs when you require one side of the body (whether front/back, left/right) to work harder in order to maintain stability;
// Progression also occurs when a proprioceptive or vestibular challenge is incorporated. This occurs following the stability challenge, e.g. standing leg press on the Wunda Chair is progressed by adding a rotator disc.
Some ideas for a pilates program with a person presenting with a gluteal tendinopathy
Step One: Building stability of the pelvis and ensuring postural patterning (when the person has a painful response to any load)
Focus
// Pelvic stability;
// Postural control particulalry of the back line;
// Isometric activation of proximal muscles;
// Good hip and shoulder disassociation.
Things to avoid
// Care with eccentric work, although those who have degenerative tendon issues could do better at this point
// Overload (monitor pain scores, above 2-3/10 cease activity or change load);
// Side lying on affected side, as may compress the bursa and common insertion of tendons;
// Compression of the glute med tendons through collapse of the pelvis and excessive adduction;
// Fatigue point where control and precision are lost.
Exercises – Example 1
Double leg focus – glute strengthening and hip flexion / extension focus. Some ideas include:
// Mini squats and sit-to-stand exercises that facilitate good pelvic alignment, postural control, flexion and extension of the hip;
// Using the wall;
// Ped-O-Pull;
// Cadillac sling support series.
The assisted squat

Gluts release with Makarlu


Hip and shoulder disassociation work, with a focus on postural strength and endurance. For example some of the exercises like:
// Knee stretch on Reformer or CoreAlign.
Exercises – Example 2
Postural focus on back line.
// Standing stick;
// Cygnet on the Wunda Chair (from the Body Organics Wunda Chair Repertoire Manual);
// Standing Arms with Ped-O-Pull or on the Trapeze Table (see the Body Organics Repertoire Manuals).
Step Two: Introduction of stability challenges (when the person is load tolerant – high load, low speed)
Focus
// Maintain pelvic stability and carefully introduce split stance work or one legged work;
// Focus on abduction control and minimise the adduction, which places further compressive forces on the greater trochanter (Grimaldi);
// Release work of the lateral line;
// Eccentric strengthening.
Things to avoid
// Side lying work that would compress the bursa;
// Fatigue point where control and precision are lost.
Exercise examples
// Single leg pump on wunda chair
// Wall ball squat
// Scooter preferably starting on CoreAlign and then move to the Reformer because the person is able to maintain pelvic stability on the CoreAlign
// CoreAlign Hoof;
// CoreAlign side standing skating;
// Four point kneeling progression to bird-dog;
// Side kneeling arms on the Wunda Chair;
// Spine Corrector side lying leg lift;
// Ped-O-Pull lunges.
Step Three: Stability challenge progression and proprioceptive challenges (when the person is load tolerant – high load, high speed)
Focus
// Maintain pelvic stability and work on endurance;
// Improve gait endurance and patterning;
// Strengthen in high and fast loads;
// Focus on abduction control and minimise the adduction, which places further compressive forces on the greater trochanter (Grimaldi);
// Release work of the lateral line.
Things to avoid
// Overload, e.g. single leg work until stability has been achieved and correct activation;
// Side lying work that would compress the bursa;
// Single leg standing work;
// Scooter on reformer, ensuring box is lined up to reformer to maintain alignment and 75 degree angle rather than 90 degree angle (as per Body Organics Reformer 1 repertoire manual);
// Standing leg press Wunda Chair (progressing to step-up a long way down the track – see the video for step-up prep);
// Step-up on the Wunda Chair;
// CoreAlign scooter;
// CoreAlign speed bump presses.
References
- Malliaras P, Cook J, Purdam C, Rio E. Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. The Journal of orthopaedic and sports physical therapy. 2015 Sep:1-33.
- Malliaras P, Barton CJ, Reeves ND, Langberg H. Achilles and patellar tendinopathy loading programmes. Sports Med. 2013;43(4):267-86.
- Longo UG, Ronga M, Maffulli N. Acute ruptures of the Achilles tendon. Sports Med Arthrosc. 2009;17:127-38.
- Longo UG, Ronga M, Maffulli N. Achilles tendinopathy. Sports Med Arthrosc. 2009;17:112-26.
- Rees JD, Maffulli N, Cook J. Management of tendinopathy. Am J Sports Med. 2009;37:1855-67.
- Cook JL, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med. 2009;43:409-16
- Louis C. et al. Strain patterns in the patellar tendon and the implications for patellar tendinopathy. Knee Surgery, Sports Traumatol, Arthrosc (2002) 10 :2–5
 0
0 
